Friday, February 8, 2008
Welcome, Doctor Anonymous Fans!
Thanks go to Dr. A for the shout-out, and Dr. Schwab for the ringing endorsement of this shabby caravansary of blogginess.
We're gonna try to blog more frequently. My goal is that for every ten words I write in someone else's comments, I'll get at least one down here.
Eric The Pragmatic
Thursday, October 4, 2007
Activity: Indoor Mini Golf

Winter is upon us, and most outdoor activities have come to an end. A great activity to provide physical and mental stimulation is mini golf (the more common term Putt Putt Golf is a protected trade mark).
We've played a couple times at Cal's facility and had a great time. The facility has an ideal layout for forming an impromptu course, with wide,carpeted non-orthogonal halls and a TV lounge adjacent to an activities room. The arrangement of the hallways and doors makes challenging dogleg holes a snap.
 Some holes can be short straight shots, while others can be doglegs with no straight path between the tee and cup possible.
Some holes can be short straight shots, while others can be doglegs with no straight path between the tee and cup possible.Encourage creativity in the game, and don't be surprised to see a bank-shot off the wall to get around an obstacle.

Objects found in the area can be pressed into service as obstacles to make the course more interesting. Two large red tulips make a nice garden hole. Do watch out for potential headaches like the opening under the TV cabinet here. Cal had three shots in a row bounce off the tulip and end up under the TV (yes, he still beat Eric and I even with a few troubles like that!).

Some objects can be added for fun, such as the big yellow bird peeking around the corner here. It came out of the bargain-bin at a crafts store for a couple bucks. A little tape and it adds a challenge and some interest to one of the holes. If people get really good at the game, you can add requirements like putting through the bird's legs. Croquet anyone?
Setting Up a Course
There is no wrong way to do this. It depends on what's available.
- The course area should be carpeted if possible. Putting will work best on a carpeted floor. Special balls are available that can be used on tile floors if required.
- The "greens" are pieces of felt roughly 3 feet in diameter. Not strictly necessary, they serve to create a more golf-course-like feel. Some are round, some oblong or kidney shaped. The shape doesn't have much impact on game play but adds visual interest.
- The putting "cups" are cheap plastic practice cups, available from most golfing supply centers for a couple bucks a piece. The white plastic or aluminum type are the best - the green ones are difficult to see on the "greens."
- The putters are the real thing, purchased at Goodwill and Value Village for a few dollars a piece. Each player should have his own putter of the appropriate length so try to find an assortment. Selecting a putter adds to the game, so having a number of styles and types makes it more fun. Note that some putters only have one face while others can be used right or left handed. Make sure to include putters that can be used either way and include some left-handed putters if you find any.
- The balls are the real thing too. Look for a colorful assortment at Goodwill and Value Village.
- The tee makers are upside-down paper bowls, with the hole numbers marked in felt-tipped pen. Position a pair of bowls about 4' apart to form the tee line.

This picture shows the first green being visited by a pair of ducks who normally live on a table. The "green" is about 3' in diameter, with the plastic putting cup near the center. The tee markers for the second hole are visible in the background.
Playing the Game
Golf is usually played with a threesome or foursome. Divide people who are playing into groups of three or four.
The first group tees off in turn, with the farthest person shooting next. The putting cups don't do that good of a job capturing the ball, so any ball crossing the center area is considered to be in the hole. If balls are close to an obstacle, they may be moved one club-head length away to allow access for hitting the ball. Part of the challenge of mini golf is playing around the obstacles, so at times, it may be necessary to hit the ball wrong-handed if it's near a wall or other obstruction. Balls that are out-of-bounds (under furniture for instance) may be moved in-bounds, no nearer the hole, with a one stroke penalty. If a tee-shot lands out-of-bounds, it may be re-hit from the tee with a one stroke penalty.
Each stroke is counted, and the player with the lowest score wins. A golf course usually has 9 holes. A game may be either 9 holes or 18 holes. Score cards can be printed on card stock, with one being used per group.

The course can range from simple to complex, and there's no right or wrong way to do it. Each time mini golf is played, the course may be set up differently and different obstacles used. The course should be set up with an eye to providing alternatives - a normal path and a bank-off-the-wall path or an option to go through an obstacle rather than around. You may see some surprising problem-solving skills in action.
A final piece of advice....someone with a closest full of golf sweaters and hats and shelves of trophies doesn't need any help. You may be amazed how well years of putting skills are retained!
Thursday, May 10, 2007
Does Anybody Really Know What Time It Is?
Reading Time Vs. Telling Time
It’s interesting to note that our grandparents, their grandparents and even their grandparents would have no trouble telling time with the analog clock on the wall. Analog clocks are essentially unchanged over the last several hundred years.
Digital clocks can into widespread use in the early 70s, with the advent of LEDs. Every digital device seems to include a digital clock these days, and unlike the clocks of many old VCRs perpetually flashing 12:00, most usually display the correct time.
Even with digital clocks being ubiquitous, the hundreds-of-year-old technology of analog clocks is still going strong. Other analog technologies, based on colors and geometric shapes, just haven’t caught on.
Reading a clock is one of the first skills we learn in grade school, and sadly one that the elderly can have problems with. Digital clocks make reading the time simple, so why haven’t they taken over?
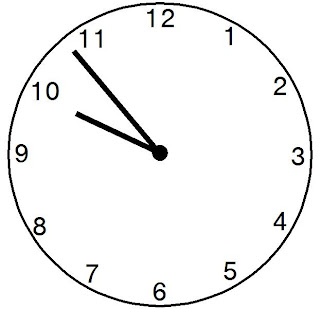
The simple fact is that reading the time isn’t the same as telling the time. Digital clocks make it simple to read the time to the nearest minute, second, or even to a fraction of a second. You’d think they’d be the ideal solution for the elderly. I know I did until recently, and only on this very day have my suspicions been confirmed. Reading the time is not the same as telling the time. Consider the two clocks shown.
From the digital display, it’s a snap to see that the time is 9:53:27. A little kid who knows his numbers can tell you this, as can most elderly folks. I’ll concede that the time shown on the analog clock is the same, but when I look at it, I see the time is nearly 10 o’clock. I know that if I have to be at a meeting at 10:00, I need to think about going. It’s simple to read the digital clock, but for the cognitively-impaired, 9:53:27 doesn’t tell them that it’s time to walk down the hall for chair exercises at 10 o’clock.
Depending on the type of impairments a person has, reading and understanding one type of clock may be easier than the other, but it’s not as clear-cut as you might initially think.
From a pragmatic point of view, I can offer a couple guidelines. When selecting an analog clock, look for a clear, high contrast face. Simple block numbers with distinct minute and hour hands. No Roman numerals and no stylized designs that omit numbers.
 For digital clocks, be wary of displays that present too much information. The time is great. Displaying the day of the week is a nice add-on. When the display includes the date, temperature, etc, etc, it becomes difficult for the cognitively impaired to pick out the time from the clutter.
For digital clocks, be wary of displays that present too much information. The time is great. Displaying the day of the week is a nice add-on. When the display includes the date, temperature, etc, etc, it becomes difficult for the cognitively impaired to pick out the time from the clutter.
Talking clocks are an option we haven't explored yet. There are some sweet clocks that can be programmed with different messages at different times of day. Another up-and-coming adventure.
Tuesday, May 1, 2007
I’d Like To Buy A Clue – Part 1

As people age, they may become less attuned to circadian rhythms and the passage of time. The elderly may not be aware of the things we take for granted, such as knowing when to get up, go to bed and eat meals.
When Cal moved to a new facility about a year ago, he went from a facility having meals at fixed, announced times to having a flex schedule for eating with each meal available any time over a two hour window. Even after much explaining, this led to many missed meals because he simply doesn’t recognize the passage of time.
To solve this problem, the “meal clock” was born. In a normal clock, the hour hand makes two
You make be thinking “great idea” but the only place you’ve seen a 24 hour clock is in Dr. Strangelove. (ok, I couldn't find a Dr. Stranglove picture including a 24 hour clock, but I'm sure there is one in the movie someplace!) It’s surprisingly easy to make a meal clock/daily reminder clock. You may have noticed that all the cheap clocks you see these days are powered by one AA battery and have a module that’s about 3” x 3” to turn the hands. 24 hour movements are available in the same package.
To build a meal clock, start with any clock using one of these standard modules. The cheapest wall clock at Ikea, the Rusch, is a great starting point.
Remove the face, gently pull off the hands and remove the clock movement by loosening the nut.
Press the movement out the back. It may be held in place with double-face tape or some locking tabs. Insert the 24 hour movement and tighten the nut. Next, replace the clock face with a new one showing meal times or other daily events. I’d recommend clearly defined and labeled areas and avoid presenting too much information. I’ve altered the traditional 24 hour clock arrangement, and made 6 AM be straight up. This means that the “day time” is shown on the right side of the clock face, evening at the lower left. Secure the face in position with double-face tape or a glue stick. Finally, install the hour hand. I cut the pointer off the second hand and installed the “button” on the clock to give it a finished look.
Setting the clock takes a little care. If possible, set it at the edge of one of the event times, at noon (straight right) or 6 PM (straight down).
Explain the operation to your loved one, showing that the hand shows when it’s time to eat or time for another activity. Don’t mention that it’s a clock as this may just lead to confusion.
This is the recently updated meal clock, with changes to reflect new meal times. The clock face is a little lighter than desired because HP wants money for a new toner cartridge. The small circles shown at 8:00, 3:30 and 8:30 PM are medication times, there for future reference if needed. The shaded area on the left side is labeled "Bed Time" - we've explained to Cal that he should be asleep during this time, and that it's not a good time to call people on the phone unless it's an emergency.
Next Time: Lighting Control Systems for Day/Night Orientation
Monday, April 23, 2007
UTI: No Laughing Matter

Urinary tract infections can have devastating effects in the elderly. Often lacking any noticeable symptoms, the results can include cognitive impairment, confusion, aggression and hostility.
Recently, Cal just seemed to be a bit off - a little more confused than normal, and struggling to accomplish tasks that usually pose no difficulty. After a week without any improvement, we had Cal pee in a cup and the lab confirmed out suspicions. Antibiotics were prescribed and an immediate improvement in cognition was noticed.
A few months ago, before we were alerted to the indications and impacts of a UTI, Cal went through a period of declining cognition, paranoia and aggression. Pill time became a big battle, with Cal denying that he ever took pills, that the doctors didn't know what he needed, if in fact they had even prescribed the pills. An hour-long battle three times a day ultimately ended with a ambulance ride in restraints to the hospital after Cal started throwing things. A UTI was discovered in the hospital.
Cognitive or behavioral changes from a UTI can occur gradually or rapidly and symptoms may not include fever, burning or frequent urination or the other conditions typically associated with a UTI. Urinary tract infections may not always be indicated by a simple "dip stick" test - samples should be sent to the lab and cultured.
Monday, March 19, 2007
Why Pygmy Bears Are So Useful In Radio Stations...
Sorry. I'm buried at work at the moment. I do have a day job...
Postings are going to be somewhat sparse for the next couple of weeks. We're working on a new version of our flagship product, and that's eating my brain. More later.
Eric
Tuesday, February 27, 2007
A Stinky Situation

Dealing With Incontinence
It's a sad fact that many people suffer from incontinence as they age. If you have any doubts, just check out the wall of incontinence products at WalMart. There are more types of adult diapers than you can imagine!
Fortunately, these products do work very well and will soak up an amazing amount of liquid. Disposable mattress pads and wheelchair liners reduce the mess if there are accidents.
The biggest problem is disposing of the used diapers; just throwing then into an open trash can leads to a stinky mess. Flip-top kitchen cans help contain the odor, but dumping the can is still not a job for the faint of heart....or nose.
A tour through the baby aisle reveals a number of diaper-containment products. None of the instructions mention adult diapers, and most of these products depend on a number of steps to spirit a used diaper safely away. For example, one type of container requires folding the soiled nappy, inserting it into the lid and twisting the lid around 3 times. The result is like a string of frankfurters... but even with rat lips and dead flys, there is no comparing this sausage to the real thing!

Our search for a good solution led us to the Diaper Dekor Plus at Toys-R-Us. This picture shows the standard model...the Plus has rectagular trap doors and is slightly larger. The instructions from the website sum it up best.
Diaper Dékor® Disposal System
The innovative Diaper Dékor is a convenient, easy and
The unique triple seal system helps to prevent odors from escaping....
sanitary way to dispose of dirty diapers. With a contemporary and hands free design, diaper changing won't become a dreaded experience. There is no twisting or turning – just step on the pedal and drop the diaper in.
The Plus size easily swallows a full adult diaper and seals it behind snap-shut trap doors and a drop down lid. It's simple for someone with cognitive impairment to use with the familiar "step on the pedal and drop it in" operation. The diaper falls into a continuous bag. After a day or two , it's a simple matter to open the door, pull out some additional length, cut the full section off and tie a knot in it. No mess, no smell and it's ready to go into the trash. The picture below shows how this works.
The Diaper Dekor Plus is allegedly widely available, but the only place we have been able to consistently find it is Toys-'R'-Us. The refill bags are not inexpensive but being able to dispose of the smell along with the diapers is well worth the expense! Remember to stock up on refills...you don't want to run out. Trust me on this.
Sunday, February 25, 2007
Slip Sliding Away....
As our loved ones age, they may become unsteady on their feet. Substantial stair rails and strategically-located grab bars prevent falls and injuries. Grab bars in the correct locations also prevent using unsafe makeshift grab bars like the bathtub faucet, glass shower doors and towel racks that fail when needed most.
Grab bars must be mounted properly to ensure safe use. Toggle bolts and molly screws can't provide enough strength - the bar could fail if grabbed by a falling person. Some builders have started to install blocking between the studs around toilets, tubs and showers so that bars can be safely installed later, but this is the exception rather than the rule.
The most common option is to locate the studs in the wall and screw the bar to the studs. At the local home center, you'll usually find an assortment of grab bars similar to those shown . For some bewildering reason, grab bars are usually available in 20" and 36" lengths. As discussed previously, studs are usually on 16" centers so the grab bars don't line up very well at all. Many people install the bars at an angle as shown so that the bar can be screwed to a stud at each end. Even this isn't a secure installation, as only 2 of the 3 mounting holes at each end can fit on the width of a stud.
Blocking might be installed between the studs so that rails can be installed horizontally and adequately secured to the wall but this requires opening up the wall. In some cases, it may be possible to go in from the other side of the wall, perhaps through the sheetrock from a bedroom or kitchen, but this still requires patching holes in the wall or even re-tiling a bathroom.
As pragmatic (and lazy) caregivers, we know there had to be an easier way. Once again, our friends at This Old House came to the rescue. Tommy installed a grab bar in a tiled tub using Wingits. So what is a Wingit? Think of a toggle bolt on steroids. Lots and lots of steroids.

The drawing shows an installed Wingit. Instead of the small contact area of a toggle bolt, the Wingit has contact over a circular area almost 3" in diameter! Each Wingit will support well in excess of 250 pounds....with a 250 pound load in a sheetrock wall, there is no damage after undergoing 1000 cycles of load application.
Wingits work with their line of grab bars as well as many others. One of the nicest grab bars is made of nylon, so it doesn't feel cold to the touch. This is what we have installed in our own shower; when you bump up against it, you don't get an unpleasantly cold clammy surprise like with a metal bar. They also look really attractive - strong like ox, but not ugly like warthog.
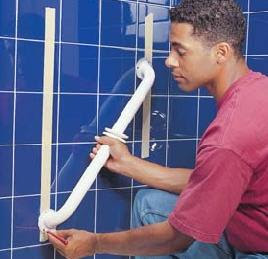
Installation is a piece of cake. As easy as pie. Determine where to install the grab bars, avoiding studs. Carefully measure the grab bar length and drill 1.25" holes using a carbide hole saw. Push the Wingit into the hole completely, allowing it to expand inside the wall. Tighten the screw. And finally. screw the grab bar to the Wingit Plate. The complete instructions show pictures of how simple this is. From start to finish, a grab bar can be installed in a tiled shower in less than 30 minutes. This is easily a quarter the time it would take to install a conventionally-mounted bar, and it is much more secure, attractive and professional-looking.
Grab bars around toilets are often helpful too. We'll talk more about that some other day.
There are many styles of Wingits available to help with all mounting needs. We recently used some light duty Wingits to mount a shelf from Ikea. They made quick work of the project.
Fiberglass Tub Surrounds and Showers
Fiberglass surrounds create some challenges to installing grab bars. With molded showers and tub surrounds, the thin fiberglass of the enclosure isn't in contact with the wall behind it. Screwing a grab bar to the studs won't work, as there may be a gap of an inch or more between the fiberglass and the wall behind it.
One innovation approach is called The Solid Mount. These mounts screw into a stud and provide an adjustable spacer to a mounting plate for a grab bar even with the surface of the fiberglass surround. The pictures show how it works.
The installation is no piece of cake, but it isn't too difficult and is far easier than opening the wall behind the tub or shower to install blocking. Use a stud finder on the wall above the surround or drill small holes just above the surround to determine the stud locations.
Other Bathroom Safety Equipment
Shower stools and chairs are handy when a loved is unsteady on their feet. They can sit down while bathing, particularly their legs and feet. A wide range of styles is available, including one from Wingits that hangs from your newly installed grab bar and lifts out of the way when not in use. A plastic patio chair may also be used in a pinch.
Non-skid mats in the tub and shower are also helpful to prevent slips and falls. Just be sure that any mat used has holes that line up with the drain so that the tub doesn't flood.
Tuesday, February 13, 2007
KISS
Keep It Simple, Stupid!
Microwave ovens are a great aid for people with cognitive impairment. They are far safer to use than a conventional stove top and quite handy to heat up a snack. Not all microwave ovens are created equal however, particularly when used by a person with some cognitive impairment.

The microwave shown to the right is typical of the kind that might be found at WalMart or Target. Lots of buttons, lots of features and really confusing to use. Even the simplest act of heating up a cup of water requires pushing a number of buttons in the correct order. If the previous cycle wasn't allowed to finish before the door was opened, more buttons must be pressed just to make hot water. Eric and I have a hard time with a similar microwave with even the basic features....and forget about the clock ever being set properly.
Cal didn't stand a chance of getting his microwave popcorn to come out right, even with a map and note to press 4 or 5 buttons in the right order!

A trip to WalMart revealed the right answer, similar to the microwave shown here. One knob sets the power level. The second knob sets the time. A few marks with a Sharpie indicate the correct power level and the proper times for some of Cal's favorite foods. Couldn't be simpler to use and it always works - sometimes some additional time is needed to get something hot but there's no frustration just trying to get the thing to turn on! And there's no clock to confuse Cal with the wrong time.
When purchasing appliances for the cognitively impaired, try it out. If you can't make it work without referring to the instruction book, chances are that it's going to lead to frustration and feeling bad. Also keep an eye out for controls that are too small to turn with arthritic fingers and labels that are too small for old eyes. Trying to make a cup of coffee shouldn't make somebody feel bad.
Down In The Dumps?

He is a clinically depressed fecophilliac on Prozac. I am just a humble pragmatic caregiver. Yet I find I should spend a brief moment on the topic of poo.
Poo is important. Not as important as some tv commercials with annoying Women Of A Certain Age who seem obsessed with poo might have you believe, but important nonetheless.
Inability to poo is a very common side effect of a wide range of medications, including narcotic pain medication, some blood pressure drugs, some cholesterol drugs, drugs for overactive bladder, antidepressants, and a literal poo-load of others. Heck, even Sudafed can make pooing problematic.
There's lots of medical references that can give you an inordinate amount of medical information about Inability to Poo. Consult them for information on various medical strategies.
One of my favorite natural interventions happens to be the unique product Fruit-Eze. It's a jamlike combination of prunes, raisins, dates and prune juice. No fancy-schmancy dried plums here. Prunes. It's a genuinely delicious combo that tastes something like the inside of Fig Newtons, albeit without the little crunchy seed bits. You can eat a spoonful of it, or spread it on toast. It's got a hefty slug of fiber in it, and is a natural source of sorbitol, a sugar-like compound that increases.....well, suffice to say, it gets things moving again.
I was first introduced to the stuff by an oncology unit nurse who looked like Adlai Stevenson with a poodle perched on his pate. She went through life with a look on her face that said "man, do my feminine organs hurt". I have absolutely nothing nice to say about this woman, given that she lacked the basic human compassion of slime mold, except for her expert advice on Fruit-Eze as a treatment for gastric quagmires caused by chemotherapy and pain medication. There, she was spot-on.
There are various recipes on the Net for "anti-constipation paste" which is essentially the same thing - a fruit paste rich in soluble and insoluble fiber. Many of these recipes contain both fruit and senna, a plant-based stimulant laxative, so be careful. It's especially important to avoid senna and digoxin at the same time. Jon was known to whip up a batch when caring for his late mother. He enjoys licking it off his fingers. He's weird.
So the next time you find that there's a pileup on the Hershey Highway, consider Fruit-Eze as a natural option to get things moving again.
Wednesday, February 7, 2007
Let's Get Physical

Apologies to Ms. Newton-John and unshod company, but I'm really thinking about physiatry, the practice of physical medicine and rehabilitation. This is not psychiatry, podiatry or psychosurgery. It's physiatry. Odds are good if someone in your life needs active care from you, they need a physiatrist too, but odds are better that unless you're a practicing physician yourself, you've never even heard of the specialty. This is a shame.
The Background:
Physiatry is really a pretty amazing specialty. Joining elements of orthopaedic medicine, physical therapy and neurology in a combo meal of medical goodness, physiatrists treat patients with everything from sports injuries to post-polio complications. I think of them as having a function analogous to an internist, but for the meat and structures rather than the squishy insides. By drawing on broad rehabilitation expertise from the entire range of physical and occupational and recreational therapists, speech pathologists, psychologists and nursing, physiatrists put people back together again, usually emphasizing a conservative non-surgical approach.
As medical specialties go, physiatry is relatively new. The first physical medicine department was formed at the Mayo Clinic in 1936, and the specialty became officially recognized in 1947. The development of the specialty is a direct result of improved survival from things that used to kill people, like major trauma, strokes and spinal cord injuries. People are living longer after body-destroying disease and injury, and physiatrists are uniquely qualified to treat these patients, often over many years.
What I really like most about physiatry is the emphasis on improving function in the face of pretty grim limitations. Aside from the sports medicine aspect (which is how I first learned the wonders of physiatry), most physiatric patients aren't going to be "cured" of their underlying conditions - the objective is to find interventions that improve their quality of life and restore as much function as possible. So if your loved one has lost a leg, a smattering of brain cells or crucial space between their vertebrae, you should probably get to know a physiatrist.
Things Our Physiatrist Has Helped Cal With:
- Alzheimer's Disease Prevention (prescribing a high-dose folate/B6/B12 supplement - I'll post on this sometime soon)
- Ataxia
- Awkward End-Of-Life-Care Discussions
- Chronic Lower Back Pain
- Constipation (physiatrists are well-acquainted with the GI challenges of the disabled)
- Exercise Programs
- Gait Issues Caused By Quad Problems
- "Mushy Hands" - mysterious hand numbness
- Neurogenic Foot Pain
- Normal Pressure Hydrocephalus rule-out
- Osteoarthritis of the Knee
- Pressure Ulcer
- Really Gnarly Fall Down The Stairs That Gave Him A Big Collarbone Lump That Will Never Go Away
- Rotator Cuff Tear #2
- Sciatica
- Shoulder Pain
- Sleep Disturbances
- Supraspinatus Tear
- Suspected TIAs/Vascular Dementia
How To Get Physical:
The American Academy of Physical Medicine and Rehabilitation is the national group for physiatrists. They have a member locator and you can find one of these amazing professionals with just a click.
Our Physiatrist:
Cal's physiatrist will be referred to here as Saint Curlilocks. It's a long story; she has overcome adversity of her own while still providing exceptional care. She worries about me and Jon almost as much as she worries about Cal. She hasn't written him off as a brain-injured old guy who can't get better, and she's open to conventional, emerging and Eastern medicine. She works us in on no notice, she can make imaging happen at the speed of light and she is well-respected by all of the other care partners we work with.
I once thought she was impossible to unsettle, utterly unflappable, but it turns out, referring to the supraspinatus as the chuck roast really creeps her out. I also find that she does not consider "trigger point injection" synonymous with "deep basting". Nobody's perfect. Suffice to say, no doctor we have ever met is even close when it comes to compassion and caring and utter dedication, but it's not just that soft squishy kumbaya stuff that we love.
Ste. C is a brilliant diagnostician, able to accurately isolate where it hurts even when Cal is at his worst in terms of cognition and communication. It's this odd combo of veterinary medicine and advanced Vulcan nerve pinch delivery (seriously, I've seen her bring an old man to his knees with a well-placed index finger - it's really amazing) that has gotten to the bottom of some problems that were really making Cal miserable. (This is not unique to her - my physiatrist has this clever little poking technique for knee pain that had me on the road to being pain-free in about 10 minutes - I think they learn secret rituals in med school). She's been able to effectively treat this crate of problems even in the face of Cal not really being a surgical candidate, being intolerant of anything stronger than Tylenol for pain and having a drug list that looks like pharmaceutical Chex Mix. She works in concert with everybody - in fact, it's Ste. C who hooked us up with our psychiatrist, even going so far as to loan out her exam room and support staff to facilitate the initial meeting.
She is our go-to gal. When was the last time you and your loved one had an hour of a doctor's undivided attention at a routine appointment? She's pragmatic, too, which of course we find adorable.
Unfortunately, we are insanely protective of Ste. C and will not tell anyone a single nice thing about her in conjunction with her real name or location, for utter fear that she will get all concerned about them and start taking such excellent care of them too, diminishing our access. So far as we claim in public, she kicks puppies, refuses to buy cookies from Girl Scouts and takes two parkings in the hospital lot. Gospel truth.
The Bottom Line:
People who need long-term management of the physical challenges of injury, chronic illness or congenital defects would benefit from the care of a physiatrist. Maybe you'll be lucky to find one as incredible as Ste C.
I Wanna Hold Your Hand...Rail


The stair rails in most homes are designed to help steady a person as they go up or down the stairs. Often, the rail is supported by two brackets, held to the wall with small screws. Brackets like the one shown can be picked up at any home center, for as little as a few dollars. Rails with this type of bracket just can't support the full weight of a person who might have a recent hip replacement or may be unsteady on their feet.
Safe stair rails and even rails in long halls and other large spaces can keep a person from falling and being injured. Searching for heavier brackets that use heavy screws to provide adequate support is an exercise in frustration. To solve the problem for my father when he had a hip replacement, we developed a method that is fairly simple to install and looks good too. We started with 2" x 6" keyhole stair rail. Lumber yards carry this, usually in cedar. To space this out from the wall, we attach a "two-by-two;" this piece doesn't show much, so can be standard grade lumber.
 The assembly is shown to the right. The stair rail is attached to the wall using lag bolts into the studs. These bolts must be long enough to thread into the studs at least 2" - be sure to allow enough length to go through 1/2 - 3/4" of sheetrock plus the thickness of the stair rail. A recess for each lag bolt should be drilled using a spade bit just deep enough so the the head of the bolt is slightly below the surface of the rail. Be sure to use a flat washer under each bolt head.
The assembly is shown to the right. The stair rail is attached to the wall using lag bolts into the studs. These bolts must be long enough to thread into the studs at least 2" - be sure to allow enough length to go through 1/2 - 3/4" of sheetrock plus the thickness of the stair rail. A recess for each lag bolt should be drilled using a spade bit just deep enough so the the head of the bolt is slightly below the surface of the rail. Be sure to use a flat washer under each bolt head.Bolts should be installed near each end of the rail, and at every other stud along the length. Pilot holes should be drilled into each stud to make driving the bolts easier and to prevent cracking of the studs in the wall. Tighten the bolts snugly but don't over-tighten the bolts or the sheetrock may crack.
Locating The Studs
The most difficult part of installing this stair rail is locating the studs in the wall. In the US, studs are usually on 16 inch centers, so finding the first one should make the rest easy. An electronic stud finder can be a great help but isn't required.
 A typical wall is shown to the right. Outlet and switch locations help us know where to look for the studs. They are usually located adjacent to a stud, so there is a good chance there will be a stud to one side. Tapping the wall with your knuckle will result in a hollow sound over the space between studs and a solid sound when over the stud. When you find one stud, measure over 16" and with a little luck you'll find another.
A typical wall is shown to the right. Outlet and switch locations help us know where to look for the studs. They are usually located adjacent to a stud, so there is a good chance there will be a stud to one side. Tapping the wall with your knuckle will result in a hollow sound over the space between studs and a solid sound when over the stud. When you find one stud, measure over 16" and with a little luck you'll find another.I like to double check the stud locations by drilling a 1/16" holes that the rail will cover to be sure I've found the center of
each stud I'll use to attach the railing. Mark the center of each stud in pencil on the wall.
The stair rail should be installed so that it's 34" - 38" above the leading edge of each step. It's usually best to install rails on both sides of the stair to have support on the needed side when going up or down the stairs.
For a guide on stair rail installation, let's turn to the pros at This Old House. A video shows the tried and true methods that Tommy Silva uses to get a perfect installation every time.

The finished stair rail will look something like this. A clear poly finish is a great look with cedar stair rail. The mounting holes may be filled with wood filler or left open for an interesting look (Eric has some other adjectives for it!)
These stair rails will support the full weight of a person without deflecting or danger of failing and provide an attractive look in the home.
Monday, February 5, 2007
Please Observe Lemurs Saucily Tangoing
In the process of transferring from the bed to a wheelchair, your loved one falls and is crying out in pain. You, being a compassionate person by nature, call 911 for paramedic assistance. Again, seems straightforward. A broken leg is a treatable condition, right?
Here's where it gets messy. In the midst of the chaos, your loved one isn't screaming anymore. In fact, they're not breathing and they have no pulse. They are quite deceased. You're clear in your mind though - no pulse, no breathing = no CPR, no intubation, no dramatic shocks from the shiny Packer Whacker . The paramedics will see the advance directive, recognize they're not needed, offer appropriate condolences and help you arrange for transport of the deceased after verifying that they are, in fact, not just resting.
Fat chance. No matter what you spent, no matter how genius your legal adviser, in most jurisdictions, your loved ones' advanced directives are not even worth the paper they are printed on in an emergency situation. EMTs and paramedics are compelled, either by law or company policy, to ignore most Living Wills and ADs. They will show up, they will see a lifeless body on the floor, and they will expressly violate their last wishes and try to make them undead again. CPR is not pretty, even when done properly.
It's probably a good idea to prevent people other than MDs from making a snap decision about who gets resuscitation and who doesn't. I'm all for erring on the side of caution in the large, theoretical way. In the intensely personal way that I view Cal, however, I'm crystal clear - ain't nobody getting lit up with enough energy to run a dozen light bulbs, even if it only takes five milliseconds.
The question is, how do we make sure our loved ones are treated appropriately in the event of an unexpected event where they can't speak for themselves?
 Enter the Lemurs (Saucily Tangoing).
Enter the Lemurs (Saucily Tangoing).You need Physicians Orders For Life-Sustaining Treatment, or the POLST. (I still think Tangoing Lemurs) Born in the early 1990s out of a frustration of healthcare ethics professionals in Oregon, the POLST is a major advance in end of life care. It provides a portable (both in the sense that it's a single sheet of paper and in the sense that it follows a patient, rather than being retained at a single facility) mechanism for a doctor to provide specific orders to prehospital responders, emergency departments and other care providers about what measures are desired and appropriate for a specific patient. In sixteen states (as of February 2007), these forms are legally binding - just the same as having the physician (or ARNP, or PA-C) there ordering the care.
The POLST is *most* appropriate for people for whom death, in a given year, would not strike a healthcare professional as a surprise. Sounds harsh, but it's an easy rule of thumb. It's appropriate for the terminally ill, those with severe chronic health problems and others for whom death is not the worst possible outcome.
There's lots of information about the POLST Paradigm at POLST.org, a service of Oregon Health and Science University. There's links to state POLST programs, an explanation, sample copies and instructions, even what color of paper to print it on to make it official. In brief....
1) Get a form. Making the effort to get the right color paper makes it more easily recognized, but copies are acceptable. Many healthcare professionals, hospitals, ambulance services, hospice organizations and state medical societies offer POLST forms at low or no cost.
2) Ponder, either for yourself or the someone you are healthcare proxy for, answers to some weighty questions, on the topics of CPR, medical interventions, antibiotics, and artificially administered nutrition (no, not like these). You do not have to be someone's Attorney In Fact to initiate this conversation. I know that broaching this topic with a loved one is uncomfortable. It doesn't have to be a big emotional discussion all at once, either - just try to get a general idea of the preferences in each category, over time if need be. Many people have expressed a desire not to be "kept alive on machines" - if you think that's the case for your loved one, you can ask clarifying questions when the time feels right. Terry Schiavo's case prompted a lot of discussion of Living Wills - if you think it's appropriate for your situation, you might use news items or events in the life of friends and family members as an aid to conversation. Note that the stock answers on the form are not the only appropriate answers; your healthcare professional can write in addenda to clarify things - in our case, we would want cardioversion to correct atrial fibrillation if the treatment is potentially curative.
3) Make arrangements to review the form with a healthcare professional. This is essential. It's the signature of someone with those special initials after their name that makes all of this stick.
4) Put the original someplace safe-yet-visible, and keep a couple of copies. We've got them in Cal's apartment, with the facility management, in his records at all of his doctors, and we just came up with the idea of keeping a copy in the glove compartment of the car we haul him around in. His non-medical caregivers and their employer have been given explicit directions around the POLST, and we've met most of the local EMS crews at one point or another, and they actually know where to look. I'll talk more about the Vial Of Life at some later date, but suffice to say, a form that is hidden in a desk drawer is effectively useless. The form will ride with your loved one to the ER if transport is appropriate, and guide their treatment there.
5) If there's been a substantial change in your loved one's condition since the original POLST was completed, consider reviewing it for appropriateness. Any willing physician can amend the orders, void a section or sign a whole new form.
We had our conversation with the doctor we see the most often, who knows Cal the best and is a great communicator. She asked him about his preferences, and guided the conversation in a way he could understand. It wasn't nearly as awful as I thought it was going to be - much, much, much easier than having the similar conversation with my mother (25 years younger, seriously ill, hospitalized with a terminal diagnosis at the time) two years before.
If your state isn't a part of the POLST paradigm yet, ask around. There may be similarly effective, portable mechanisms for specifying care preferences. Hospice organizations can be especially helpful in this regard.
Tangoing Lemurs. Seriously. Get you a POLST and sleep better at night, knowing that your loved one is more likely to get the exact end-of-life care that is best for them.
Eric
prag-m&-tik
Practical; concerned with making decisions and actions that are useful in practice, not just theory.
Way to go, Wiktionary. Nailed it.
I'm Eric, one of the two Pragmatic Caregivers. We're two guys, with absolutely no academic or professional qualifications whatsoever, who have been thrust into the role of caregiver for an 84-year-old parent, who will go by the pseudonym Cal. (But I swear, we really are Eric and Jon.)
Four years ago, Cal had a bad surgical outcome - he went from being an independent 80 year old with orthopaedic problems and the various frailties of aging to someone who was no longer able to live safely and comfortably in an independent manner. Quite literally overnight we had to go from being concerned adult children to active managers of virtually every aspect of his life. We knew *nothing*, but we both take a very practical, results-driven approach to every other aspect of our lives, and thus, we learned on the job.
Here, we will present some of our random musings - things that work, things that have not worked, things that we're working on. We don't make any money from anything related to caregiving - our business is geeky in the best possible way and we're really proud of what we do, but the commentary here is absolutely 100% free of crass commerce - and if we mention a specific product or service, we'll explain our relationship to the organization, which will probably range somewhere on the scale from "totally satisfied customer" to "preparing pitchforks and burning torches to storm the headquarters".
We'll periodically exercise our editorial prerogative and comment on emerging science, various clinical innovations, bad science in media and whatever we think might be useful.
Eric